The Catch-22 of Limiting PFAS Exposure
Welcome to the fourth issue of ContamiNation. Subscribe for free to receive it monthly, and please share this newsletter with others.

If you’re fortunate, your primary care provider might follow the guidance of the National Academies of Sciences, Engineering and Medicine (NASEM) and inquire about your exposure to per- and polyfluoroalkyl substances (PFAS). Assuming you don’t have high occupational exposure or drink from a well at risk, your clinician might conclude the exchange with encouragement to limit PFAS exposure where you can.
Individual risk reduction is essential but inherently problematic. It keeps the focus on adapting to the status quo when there’s an acute need to reduce PFAS at the source—limiting the production and use of these pernicious chemicals.
Do-it-yourself fixes unfairly burden those who did not create this problem. Why should the onus be on them to research and purchase water filtration or replace consumer goods that hold hidden hazards?
Personal risk reduction also favors those who have time to educate themselves and the resources to take protective measures. Many of the people most vulnerable to the ill effects of PFAS don’t have those advantages.
The NASEM Committee report on PFAS captures the irony at the core of individual interventions: “Reducing intake of PFAS should reduce exposure, but people may not necessarily know whether their foods, beverages, or products contain PFAS.”
That’s the Catch-22 we all face: How can we limit PFAS exposure when we don’t know where these chemicals are found? PFAS can lurk in the water and food we chow down and in the products we slather on, pop on our eyeballs and pull through our teeth.
We know that PFAS enter our bodies through some combination of ingestion, inhalation and dermal absorption, with the former often deemed the dominant route of exposure. But with all three pathways, there’s insufficient data to guide efforts at lowering risk.
Progress is happening in testing public water systems, but no state has committed to underwrite the testing of private wells (which supply up to half of households in some rural states). So the breadth of exposure to contaminated water—likely one of the greatest health risks—is still unknown.
Research on where PFAS concentrate in foods is still embryonic, making it hard to know what to avoid.
For consumer goods, where a single study identified 200 product categories likely to use PFAS, there are no product databases and the one online listing of PFAS-free products includes just 10 categories.

In cases where product testing has occurred, such as the work Consumer Reports and other researchers have done to assess takeout packaging that can leach PFAS into food, there’s still a huge onus on consumers to track that research and keep up with the latest developments on which claims about PFAS-free packaging hold up (spoiler alert: not all of them do).
That’s why a dozen states have now moved to restrict PFAS in food packaging, while a smaller number are phasing out PFAS use in other product categories such as apparel, carpeting, cookware and ski wax.
Only two states have committed to phasing out PFAS across all product sectors except when uses are deemed essential. A critical first step in that process requires that retail businesses report on which of their products contain PFAS. Maine has begun that challenging process, and Minnesota is following suit, with “Amara’s Law,” which requires reporting on PFAS in products by 2026.
Maine’s work to trace the whereabouts of PFAS demonstrates that consumers aren’t the only ones in the dark. Many retailers have no clue which of their products contain PFAS. Even manufacturers of those products often plead ignorance, pointing up the supply chain to chemical corporations that may assert such information is “proprietary.”
Tracking stealth chemicals that we cannot see, smell or taste requires transparency in production processes. Without comprehensive reporting of PFAS, we can’t begin to get a grip on this insidious contamination.
The medical counsel to “reduce your PFAS exposure” is sound advice. To follow that prescription, we need for businesses at every level to reveal how and where we’re being exposed.
]
Research: Discovering the Impacts of PFAS in Pets
Until recently, there has been little guidance the veterinary field could offer to members of PFAS-affected households concerned about how the chemicals might harm their companion animals. That informational void is starting to fill as researchers in North Carolina and Michigan examine dogs, cats and horses with heavy PFAS exposure.
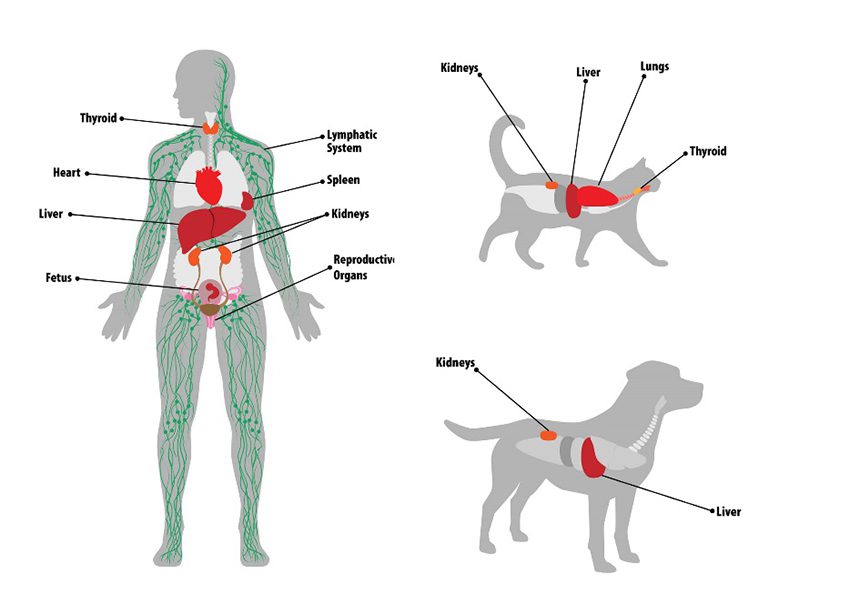
Companion animals are better able to excrete PFAS than people are; compounds that might linger in humans for years or even decades appear to stay in these pets less than two months. But dogs and cats do show some health effects similar to those humans experience—with impacts to the liver, kidneys and—in cats—the thyroid.
Responding to community concerns near a notorious Chemours fluorochemical plant, North Carolina State University researchers tested for 33 different PFAS in the blood serum of dogs and horses living on properties with PFAS-contaminated wells. More than half of the 31 dogs and 32 horses had at least 12 of the 20 different PFAS found, and every animal had at least one chemical. Dogs given bottled water had different PFAS than those drinking well water, suggesting additional exposure pathways such as household dust.
Impacts from contaminated water, soil, air and dust are complicated by PFAS exposure pets can get from commonly used flea and tick products. Grease-resistant pet food packaging can also be a potential source of PFAS.
Horses in the study had lower concentrations overall than dogs and a smaller range of PFAS compounds in their blood serum. Clinical check-ups of the horses and dogs revealed some indicators of kidney and liver issues.
Median concentrations of two PFAS compounds found in dogs were similar to levels found in a regional exposure study of children, suggesting that dogs could potentially be “sentinels,” helping to signal where PFAS levels are elevated.
Research led by Heather Bair-Brake, a veterinarian and graduate student at Michigan State University, supports the finding that blood serum levels in dogs and cats are often analogous to those of humans living in the same community. Pets may be an especially good indicator of PFAS exposure in children (who, like dogs, tend to spend more time on carpets and floors and put items routinely in their mouths).
The Michigan research study, slated for completion in 2025, may yield more information on how pets get exposed to PFAS, how long various compounds remain in them, and what levels of exposure prompt adverse effects. The study’s next phase will look at whether certain blood values change when pets are exposed. “If there are consistent changes in the blood work of exposed pets,” Bair-Brake notes, “veterinarians may be able to determine contamination in the household by interpreting those differences.”

News of Note
Following a staged ban the European Union enacted last fall on the sale of microplastics and products with intentionally added microplastics, researchers at Yale School of Public Health and other institutions are calling on other nations to adopt this step. The U.S. has banned plastic microbeads in many ‘health and beauty’ products, but not the microplastics used in liquid detergents, paints, agricultural products, pharmaceuticals, and artificial turf.
A small-scale study offers further evidence that sewage sludge applied to agricultural lands spreads —not just PFAS as Maine has documented—but microplastics. The research found that wind-blown sediments from sludge-treated fields contained a higher concentration of microplastics than either the sludge or the soil, due to the plastics’ lighter density and their capacity to resist soil moisture. Even breezes gentle enough not to stir up dust sent microplastics airborne, they found.
Chemical additives in plastics, many of which may hitch a ride on nanoplastics into our bodies, carry high health costs, a new study finds. The Los Angeles Times summarizes the work conducted by researchers at New York University, Children’s Hospital of Philadelphia and the Maine nonprofit Defend Our Health.
Researchers at the University of Southern California found in a cohort study of young adults that PFAS blood levels rose over time among participants who ate more processed meats, drank more tea and consumed more foods prepared outside their homes. The study authors noted that their findings confirm the importance of states requiring manufacturers of food packaging to disclose PFAS in their products.
The EPA has taken steps to require reporting from businesses that import or manufacture PFAS, and to advance regulation of nine PFAS compounds under the Resource Conservation and Recovery Act. A summary of these new measures appears on the Substack newsletter of environmental scientist Mindi Messmer.
Good Resources
The Safer States 2024 PFAS Policy Toolkit provides an informative resource for advocates, legislators, journalists and concerned citizens interested in learning about PFAS-related policy measures. The nonprofit organization Safer States also tracks proposed legislation on toxic chemicals, and estimates that at least 16 states in 2024 will introduce broad measures on PFAS in products.
“The Poison in Us All,” a 48-minute Bloomberg documentary, introduces PFAS concerns to those not familiar with their risks.
Thanks for reading!

